Original Article: DNRs and Advance Planning for Kids: Everything You Need to Know
If your child has a life-limiting condition or has experienced severe illness in the past, you may have strong opinions about what types of interventions you want if your child becomes critically ill. There are many methods of conveying your wishes for your child, using a variety of physician orders or legal forms, including DNRs, DNIs, ANDs, POLSTs, Advance Directives, and Advance Care Plans. How do you know which one is right for your child?
In this article, we will go through all the various acronyms, explaining the pros and cons of each type of advance planning order or form, including how each will be interpreted in a variety of settings.
The Worst Plan: Not Having a Plan
No matter how significant or insignificant your child’s issues, you should always have a plan. That plan may include full CPR, intubation, mechanical ventilation, and all other medical interventions. Or it may include comfort measures only. What is important is to develop a plan for your child and let his or her medical team know that plan. If your child will be receiving full interventions, you typically do not need to create a formal plan. But if you plan on restricting any interventions, it may be wise to engage in advance planning.
While putting a Do Not Resuscitate or similar order in place is of course an individual choice, in general, children with stable disabilities should not have one if they are expected to live for many years with no worsening in their disability. These families might consider an Advance Care Plan instead, which is an informal document that states the family’s preferences if the child’s condition changes or worsens. Do Not Resuscitate and similar orders are only appropriate for children with life-limiting conditions who are expected to decline or are nearing the end of their lives.
The sections below will outline the many options for developing a plan that restricts medical interventions for your child.
Abbreviations
When it comes to the alphabet soup of advance planning acronyms, one can get very lost between all the various letters. Here’s a simple guide to the most common names for advance planning orders and forms.
| Acronym | Meaning | Order/Form | What It Is |
|---|---|---|---|
| DNR | Do Not Resuscitate | physician order | No CPR and typically no intubation |
| DNI | Do Not Intubate | physician order | No intubation; may include no CPR at some facilities |
| AND | Allow Natural Death | physician order | Usually no CPR or intubation |
| POLST (MOLST) | Physician (Medical) Order for Life-Sustaining Treatment | physician order | Varies depending on the contents from full CPR to full DNR |
| ACP | Advance Care Plan | varies | Varies depending on the contents |
| AD | Advance Directive | legal form | Varies depending on content; 18 and up only |
Physician Orders Versus Legal Documents
In general, there are two different types of advance planning documents: physician orders and legal documents. Traditional DNR, DNI, AND, and POLST documents are virtually always physician orders. This means that your child’s physician fills out and signs the relevant form stating what your child’s advance planning consists of. Any medical professional, including Emergency Medical Services (EMS or paramedics) and home nurses, must abide by what the physician has ordered as long as they have the form in hand.
By definition, Advance Directives are legal documents. Each state has specific guidelines (and in many cases, specific forms) for creating Advance Directives. These documents can only be created for individuals over the age of 18 who are mentally capable of understanding and signing the forms. They typically include the designation of a health proxy (someone to make medical decisions for you if you are unable to do so), as well as a living will or other document that includes your wishes for life-sustaining medical treatment. Because Advance Directives are legal documents and not medical orders, Emergency Medical Services, schools, and other non-medical facilities cannot—and will not—honor the decisions made within the documents. They will only be honored once a patient has been stabilized in a medical facility, such as an emergency department. This means that paramedics will always perform CPR and intubation, if necessary, even if Advance Directives are in place.
Strictly speaking, children are not eligible to have legal Advance Directives, as these are legal documents only for adults, and most typically used for future planning in that population.
Children are able to have Advance Care Plans, which are comprehensive plans typically created by a healthcare facility or palliative/hospice program. These vary in nature, and may include physician’s orders as well as informal guidelines for care planning. They typically are not legal documents, though some may include formal Advance Directives for people over age 18.
The Problem with a Basic DNR for Children with Complex Medical Needs
Currently, many children with severe, complex conditions are given a standard or basic Do Not Resuscitate (DNR) form. This form, which may be a hospital-created form, a hospice-created form, or a standard statewide DNR order form, includes only one option: in the case that the patient stops breathing or the patient’s heart stops beating, CPR should not be attempted. In many facilities, a basic DNR order also will mean a patient will not be intubated.
Example 1: Virginia Basic DNR Form
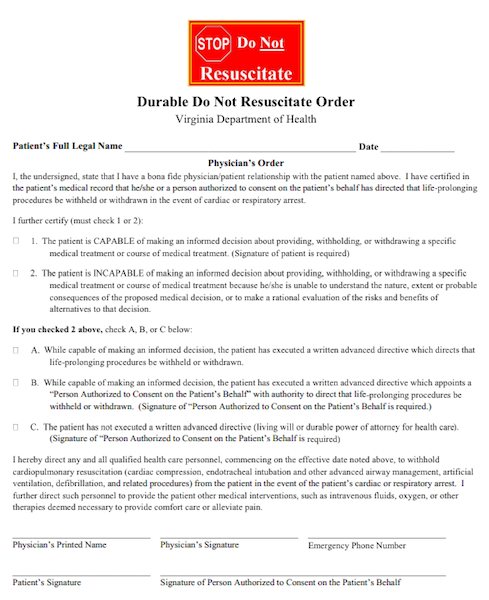
There are typically two types of DNR forms: an in-hospital DNR form that applies only within the hospital, and a pre-hospital DNR that is in effect at all times for a given child. In most cases, a child will have both a DNR on file at the hospital, as well as a second pre-hospital form that he/she will keep on hand at all times.
The problem with a standard DNR is that it often doesn’t work well for children who have complex medical needs. Let’s take a look at two potential vignettes:
A child with a trach may have mucus plugging and can stop breathing if no intervention is performed. For many children, mucus plugging is a frequent occurrence that is easily resolved by suctioning and a few breaths from a resuscitation or Ambu bag. How is a DNR interpreted for this child? If breathing stops but can be re-established with suctioning and an Ambu bag, should suctioning be attempted? Virtually all parents and physicians would say suctioning should be performed, but technically the child has stopped breathing, and an individual like a school teacher could reasonably make the decision not to suction because the child has a DNR in place and has stopped breathing.
A child who is in an accident may require intubation due to broken bones in the face or neck. This child may need brief intubation while the bones set or heal, but will otherwise not be affected by the injury. Many parents would want to intubate in such a situation. However, with a DNR in place, medical personnel may not intubate, allowing the child to die.
Many parents do not think through these types of possibilities when creating a DNR, as they are focusing on a major, life-altering episode. However, it is possible for a parent’s intention in creating a basic DNR to be misinterpreted, especially by non-medical people, since the language in most basic DNRs is so black and white.
A DNR order can always be rescinded, even on the spot at the time of the event. If the parent or guardian is not present, however, he/she cannot rescind the order in the instance of an unusual or vague situation like the two previous vignettes.
In general, simplified DNR, DNI, and AND orders that are not specific should not be used for children with complex medical issues living in the community, as the complexity of their issues makes it difficult to know when to intervene. The exception, of course, is a child in the hospital with a defined critical illness, or a child on hospice who is nearing death in a somewhat predictable way.
POLST: A Better Option
A better option for children with complex medical needs is the use of a POLST form, sometimes also called a MOLST form. These forms are like a basic DNR, but include more options within the spectrum of interventions. POLST forms are reasonably standardized, and are currently used in all but seven states. Some states exclusively use POLST forms in lieu of basic DNR forms, though hospitals and facilities may continue to use their own forms. In other states, POLST forms are one of many available options.
A POLST form always travels with a patient and is in effect at all times, in the hospital or outside the hospital. A POLST can be rescinded or changed at any time, including at the moment it would be put into action.
Example 2: Illinois POLST Form
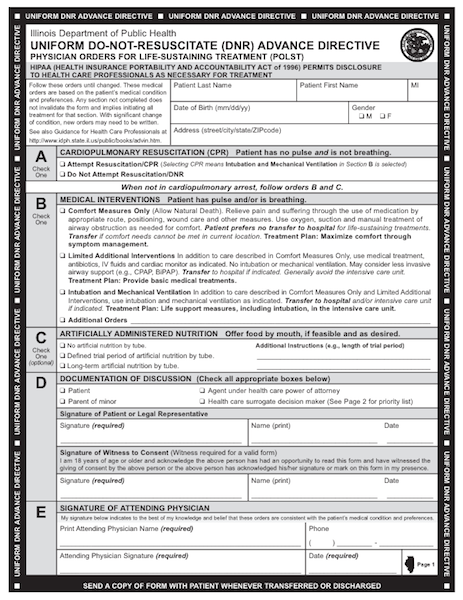
A typical POLST form allows an individual to elect to have or decline CPR when there is no pulse and no breathing. If the patient is breathing or has a pulse but a major medical issue arises, you may elect to use comfort measures only, limited interventions (such as antibiotics and IV fluids), or use full interventions, including intubation. A section on tube-feeding and/or IV fluid and nutrition is usually included. This allows more specific and appropriate choices for children with complex medical needs.
One limitation of the POLST form is that it does not work well for children who already receive major interventions, including children with feeding tubes, children on IV nutrition, and children with trachs and vents. These children may not easily fit into the defined categories on a POLST form. Nonetheless, a POLST form gives much more specific information that will better guide medical and non-medical personnel in caring for your child. For more information on POLST forms, see the National POLST Paradigm.
Advance Care Plan: The Best Option
The best possible option for children with complex medical issues is to develop a comprehensive Advance Care Plan, which may include both legal forms and physician’s orders, as well as other more informal planning.
For children with chronic and stable issues, the Plan may only include general information about future wishes. Typically, these instructions parallel adult Advance Directives (though they cannot be legally defined as such), and are not physician orders. If the child becomes ill in the future, these future wishes can be put in place in the hospital setting, or converted to a physician order.
When a child is declining and expected to eventually pass away, however, the Plan will often include a POLST form or similar other physician order, which may be hospital or state specific.
In some cases, an Advance Care Plan may actually simplify a standard DNR, such as restricting it to no chest compressions if the patient has no pulse.
In other cases, the Advance Care Plan may address specific scenarios that may occur, such as the need for a patient with a trach to be placed on an oscillating ventilator, and create specific plans for each scenario. Some institutions and programs allow families to be extremely specific about which interventions they wish to use, and which they wish to withhold.
Examples of specific scenarios might include some of the following:
- Do not initiate chest compressions or defibrillate. Medications may be given to increase blood pressure.
- If the child (with a preexisting trach) suffers a respiratory decline and stops breathing on his own, he may be placed on a standardized ventilator for a period of up to 4 weeks. He may not be placed on an oscillating or other specialized ventilator, receive medications to sedate/paralyze, or receive ECMO.
- Intubation only in the case of a self-limited illness or accident.
Depending on how the Plan is created, it may or may not include an official medical order. If any component of the Plan is not an official pre-hospital medical order, emergency personnel will not be able to follow it, and will initiate CPR.
Most palliative care programs and programs for children with complex or special needs can help you develop an Advance Care Plan. Other general pediatricians and specialists may also be able to help you create one.
Example 3: Maryland Comprehensive MOLST form

DNRs, POLSTs and Schools
Unfortunately, many schools simply refuse to honor DNR or POLST orders, even if they are written as signed physician orders or a standardized state form. In some locations, state, local, or district rules prohibit the implementation of DNR or POLST orders. In other locations, school districts have determined that they do not want to be liable for knowing when an order should be implemented.
If your school district does allow DNR or POLST forms to be implemented, be very cautious in how your orders are written. The school staff is not trained to assess and make medical decisions regarding a child’s medical status. Even a school nurse may be unable to make these decisions. If the orders are not written very specifically, they may be implemented erroneously. The previous example of a child with a mucus plug that could be resolved with suctioning and a few breaths from a resuscitation or Ambu bag is a prime example. School staff could easily misinterpret the situation and fail to intervene in an easily resolvable situation. This is why it is extremely critical to have detailed plans that clearly specify if and when interventions should or should not occur.
For more information on DNRs and POLSTs in the school setting, see this position statement from American Academy of Pediatrics.
Plan Ahead!
It is always difficult to have discussions about end-of-life and resuscitation orders. But if you want what is best for your child, and want control over what will and will not be attempted, it is critical to have a comprehensive Advance Care Plan in place. Ultimately it will protect your child, both from unwanted interventions, and from individuals failing to intervene when they should.


































Recent Comments