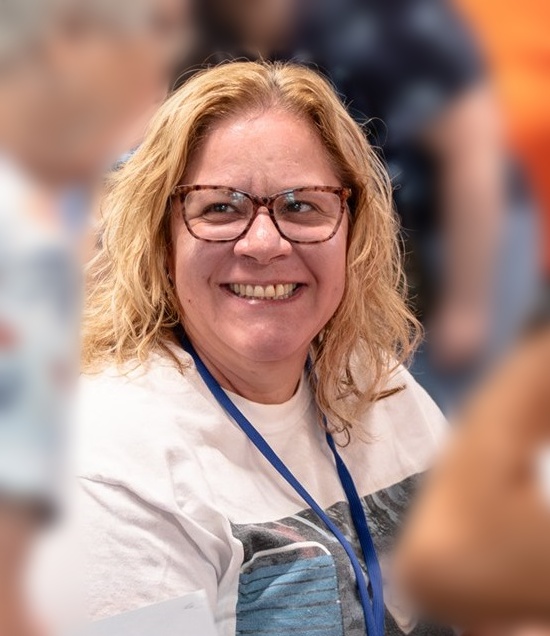
Birth Plan for Hannah Faith, diagnosed with Trisomy 18
On October 7th 2013, I was 14 weeks pregnant and expecting a call from our genetics counselor to reveal the gender of our third child! Her words, instead changed the course of my life. My child had Trisomy 18. I had never heard of it. But even as she still was speaking, I began googling and was confronted with phrases such as, “50% of babies who are carried to term will be stillborn” or “less than 10% survive to their first birthdays” My heart sank. The counselor asked me if I wanted to know the gender and I was shocked because that was my initial reason for wanting the call. I later realized that some people didn’t want to know the gender, because it would make the child they were about to abort more real. We had known from the outset that wasn’t an option for us.
We were having a second girl, what I had secretly hoped for. My heart broke with the knowledge that I
had to call my husband and tell him the news. One of our first tasks was giving our daughter her name.
We wanted to establish that she was a cherished and loved child. Unique and individual. She wasn’t
‘the fetus with trisomy 18’. She was our daughter, a sister, a granddaughter. She was Hannah Faith.
We had always known we would give our second daughter the middle name ‘Faith’ and it was singularly
fitting for our Hannah. We wanted to stress her humanity to her doctors. We wanted them to
acknowledge her as a human being with her own right to be her best self.
Learning all I could
From that day forward it was my job to learn everything I could about Trisomy 18 and its associated
anomalies so I could be my daughter’s best advocate. Google became my new best friend. From the
beginning I was drawn to the medical journal articles because they had the most fact based information.
To start with I wanted to understand the accuracy of the screening test I had taken. We didn’t have an
official diagnosis yet, just a screening test that had a very statistically low false positive rate.
During my personal research, I discovered a phenomenon called ‘confined placental mosaicism’. That’s where the screening test says you’re positive for a trisomy, but it’s only the placenta that has it. My logical side told me it was highly unlikely that we had this, however my hopeful side said “but you could…”.Because we had declined amniocentesis, our next sonogram would most likely confirm the chances of mosaicism if Hannah had any sonogram markers for Trisomy 18. I began researching potential markers and anomalies in preparation for this sonogram. I had bought a notebook that fit easily in my purse and called it my Hannah book. It was where I could scribble medical details or a question when I thought of it.
We had this sonogram with the perinatologist at 18 weeks gestation. On this first appointment after
receiving the screening test results, the sonographer walked in with the perinatologist and the genetic
counselor. I was happily surprised that the doctor didn’t make us wait to find out what was going on.
This was my first sign that this was the right doctor to follow Hannah and manage her care in utero. As
the sonographer went through her routine, the doctor told us what she saw. I interjected questions as
an area was reviewed that showed up on my list. After about the third interjection my doctor said
“You’ve done your research, haven’t you”.
My husband’s favorite moment was at the end of the appointment when I tried to say polyhydramnios and the doctor and genetic counselor both said “excess fluid”. But it was important to me to know the words that the professionals used, and to show the doctors that I took an avid interest in what was going on, I wanted to be able to understand their language, and I wanted them to know I would be doing independent research so I could ask intelligent questions. Unfortunately at that appointment we saw that Hannah had bi-lateral choroid plexus cysts (CPC), which are small pockets of fluid in the brain that most often resolve before birth. While many unborn children have CPCs at some point in their development, they are a particularly telling indicator of Trisomy 18. The combination of the screening test and the CPCs confirmed for us that Hannah did have Trisomy 18.
During the next several weeks of our pregnancy I was reading everything I could get my hands on about
Trisomy 18. I discovered that SOFT USA (www.trisomy.org) and the International Trisomy 13/18 Alliance
(www.internationaltrisomyalliance.com) have a repository of summarized research publications. I saved
these articles and started two folders on my computer. One named “Trisomy 18” and one named
“Hannah”. It was important to me that I put my research in the Trisomy 18 folder and the pictures and
videos in Hannah’s folder. While Hannah has Trisomy 18, it’s not what defines her…it’s just part of her.
Each article added to my understanding not only of Trisomy 18, but also the prevailing attitudes of
medical professionals.
One of the first articles I read was ‘The Trisomy 18 syndrome’ by Cereda and Carey. The first time I read it my eyes were filling with tears, looking at the details of what Hannah would be faced with and then I read the caption to one of the pictures “Note the characteristic hand feature with the over-riding fingers, the tracheostomy, and his engaging smile.” His engaging smile…I audibly gasped and was filled with joy that someone recognized this child’s smile in addition to his anomalies. It gave me hope. My other lifeline was online social networks filled with parents whose children also had been diagnosed with a Trisomy. The importance of social networks was even identified in another one of the journal articles I read early on ‘The Experience of Families With Children With Trisomy 13 and 18 in Social Networks’. Banding together to share experiences with other parents and pool our knowledge was a critical element in preparing and comforting me as I came to grips with my new reality.
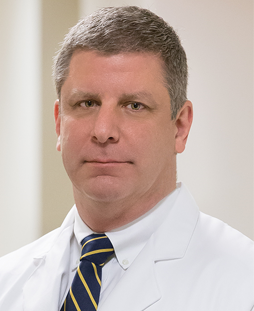
Going through the journey of a high risk pregnancy, I wound up seeing a team of doctors. I had a
perinatologist, obstetrician, cardiologist, and a palliative care doctor. Each one brought something
different to the table as we went on this journey together. My obstetrician remained my primary care
provider throughout the pregnancy. When we first found out about Hannah’s condition I immediately
made an appointment with her. She was so warm and caring, but also so sad. She’d only delivered a
few babies with Trisomy 18, and none of them made it out of the delivery room. By the time my next
regularly scheduled appointment came around I had my list of questions ready. We talked about what
labor would look like. My doctor suggested I would labor naturally with intermittent monitoring of her
heart so we would be aware if she passed during labor. At this point I was just taking everything in, so I
didn’t push for anything different.
I asked for recommendations on the purchase of a fetal Doppler at home because I wanted to be able to hear Hannah’s heartbeat whenever I wanted reassurance. Instead my doctor handed me the one out of her pocket. She wanted to make sure I had reliable equipment. She also gave me the range of normal heart rates. If Hannah’s got too fast or too slow I should call the office. The Doppler was very comforting for me throughout the pregnancy. Every morning before we left for work and while our older children were asleep, my husband and I would have our Hannah time. We would talk to her, tell her we love her, and listen to her heartbeat. At the beginning, before I could feel her move, it was quite nerve wracking…never knowing if this was the moment we would lose her. I continued to see the perinatologist regularly. At the 20 week sono we were able to get a good look at her heart and to our surprise and delight, they didn’t see any issues with it. This is particularly unusual because 80% of children with trisomy 18 have heart defects. In fact, in order to be prepared for this appointment I had combed through various journal articles to see what the common defects were. Then, in an attempt to understand them, I googled images for each one. Some were easy once I understood what the 4 chambers of the heart were named, but others were much more complex. So much so that I made a powerpoint file of good pictures of each defect so I would have a visual aid my doctor could use to help me understand the defect once we knew which one Hannah was affected by. I was very happy to tuck that file away in my archives.
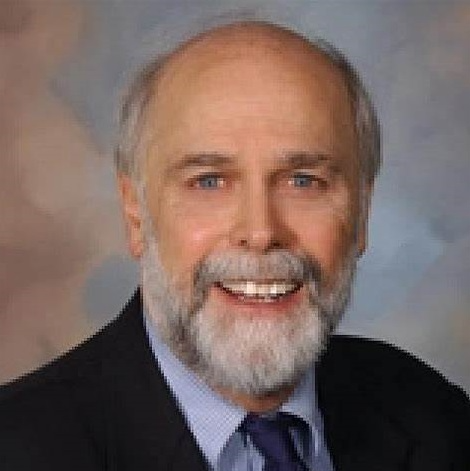
Also at the 20 week appointment we met with the palliative care doctor for the first time. This doctor’s only goal was to help us figure out what level of care we wanted for Hannah once she was born. There were a lot of tough decisions to make. We talked about what level of resuscitation to do for Hannah. Were we going to do chest compressions? Chest compressions can cause significant pain for the recipient, did we want Hannah to endure that pain? Were we going to allow her to be intubated and put her on a ventilator? Which would often mean we couldn’t hold her while she’s intubated. Were we going to put her on a CPAP machine that would allow her to breathe easier with pressurized oxygen by keeping her airway open? CPAP would necessitate her going to the NICU, did we want to be separated from her? What if she didn’t nurse well from me or from a bottle? Did we want to tube feed? What if her body couldn’t process food, which happens in people whose end is near and their body is shutting down. The list of care decisions along with their pros and cons was daunting and necessitated another more specific round of googling, reading and learning.
At this point the only thing we knew for sure is we didn’t want her put on a ventilator because we
wanted to be able to hold her. We wanted to always be able to be with her and to baptize her
immediately if there appeared to be any signs of distress. We left the meeting with lots of questions.
The palliative care doctor was going to send us some articles to read to help us reach our decisions. One
of the biggest points we got from this meeting was that we felt Hannah would declare herself. Hannah
was going to tell us if she was a fighter and a survivor, or if living outside of the womb was just too much
for her. It was our job to educate ourselves on all the options and interventions and then follow her
lead after she was born.
Meanwhile, I was making contacts at the hospital I was going to deliver at. While this was my third
child, it was the first at this hospital. I had no idea what their policies, procedures, or logistics consisted
of. The thought of going on the standard hospital tour was emotionally too hard. The questions I had to
ask were not appropriate for that audience. I cold-called the labor and delivery desk and asked to talk to
the charge nurse. This was one of the best moves of the entire pregnancy. The charge nurse invited
Jason and I to come up and she would answer any questions we had. When we arrived she showed us
around the labor & delivery floor. She answered all of our questions, including the tough ones about on
what were the procedures if Hannah was born still. She invited me to come back once I had preregistered so we could put as much information in the system as possible so there would be fewer questions on the day we came to deliver. She made us feel welcome and that we were going to be taken care of. It was one less burden for me to bear. Most importantly it got the nurses that would be in charge of her delivery invested in Hannah, in her life, and in our family. We weren’t just another labor off the street…this was Hannah and she was going to have some challenges, but we were going to do everything we could to make her life the best possible, no matter how long it was.
At my next obstetrician visit, at 21 weeks, we were thrown for a loop. We had requested a sonogram
with every visit in order to see Hannah as much as possible, and my doctor happily obliged, however this
sonographer saw something wrong with Hannah’s heart. She thought it looked like one of the more
severe defects. It was so hard to hear this considering the perinatologist had just given her heart a clean
bill of health. I called back to the perinatologist’s office and got a follow up appointment as soon as
possible. My regular perinatologist was out of town so her partner looked and she didn’t see anything
wrong with her heart. Because of the differing opinions we decided to enlist the help of a specialist, the
pediatric cardiologist.
The cardiologist looked all around at Hannah’s heart. Her sonogram machine was better, and her sono tech did nothing but look at hearts. They spent over an hour taking pictures and trying to get Hannah into the best possible positions and though she couldn’t rule out a small hole in the bottom two chambers of her heart, she didn’t think there was one, and what she was seeing was a limitation of the sono machine. So we put the fears of a heart defect to bed and kept marching on. We also decided to stop getting sonos at the obstetrician’s office. We were seeing Hannah plenty of times at the perinatologist’s office and we didn’t need the stress of one person seeing something that the other did not. We trusted the high risk doctor to see anything we needed to know.
Our next curve-ball came at about 26 weeks. At about 24 weeks gestation, the babies umbilical cord
blood flow can be measured and is a good indicator of the babies health. At Hannah’s first blood flow
check, the high risk doctor saw no issues but this time she saw something concerning. We were looking
at the S/D ratio (systolic/diastolic). It is measured by the sonographer taking readings of the blood
flowing through the umbilical cord. This can be particularly challenging if you have a squirmy baby, but
it is vital to helping understand if there is appropriate blood flow through the umbilical cord. Hannah’s
ratio was elevated at 6.1 and it wasn’t supposed to be above 5 at that point in the pregnancy. We
needed to keep an eye on it because if it got worse we would start seeing absent end diastolic flow or
reverse diastolic flow. Both of these are indicators of imminent fetal death. This made me incredibly
nervous because I had met another Mom online whose daughter was named Hannah Faith and they lost
her due to poor umbilical blood flow. My doctor said she would see me in two weeks to monitor again.
I didn’t last the two weeks. I got nervous and wound up in her office a week later. Hannah looked great,
and I felt better knowing she was still ok. Together we decided that getting checked once a week would
help keep me sane. My doctor was so amazing. Her focus was helping to get Hannah here alive and to
keep me as calm and together as possible. If that meant I came in more often than she felt we needed
to check Hannah she was always willing to defer to my request.
Because of the compromised blood flow, it was time to start discussing the delivery method. My high
risk doctor told me that in these cases, she recommends a scheduled c-section. During contractions,
blood flow through the umbilical cord is reduced and since Hannahs flow was already compromised it
could put her in to distress. As a momma who had 2 children naturally with no medication, the idea of a
c-section was incredibly scary, but knowing it would give Hannah her best chance I was 100% for it. The
question was would my OB agree to it. Then next time I saw her we talked about what was going on and
she said most definitely we should do a c-section and get this little girl here in her best shape. But then
came the tightrope walk. With the compromised blood flow, which the s/d ratio indicated, we would
likely need to deliver her early, but how early? She wanted us to start checking her heart beat twice a
day using the home fetal Doppler she had lent to us. If it started slowing or falling below her lower
threshold (110 beats per minute for Hannah) we would need to deliver. At the same time, we wanted
to let her grow and develop as much as possible, because the older the baby the better the chances.
She recommended delivering sometime between 35-37 weeks if she made it that far. It was pretty
awesome to see the change in my OB. While she supported us whole-heartedly from the beginning, she
didn’t think Hannah would make it this far. She said every week she kept waiting to get the call from us
that she was gone. But seeing how strong she continued to be, she felt that we were going to meet
Hannah alive.
Another great benefit of listening to her heart beat in the evening was allowing our big kids to get to
know her while in utero. Every night we gave “the bigs” the option to listen to Hannah. My 4 year old
decided that she needed to talk in to my belly button to tell Hannah she loved her. Even the 2 year old
got into the spirit of it and would give Hannah kisses through my belly. It was precious family time and I
was so hopeful that this wouldn’t be the only time we had together as a complete family of 5.
Because we were now on the c-section path I wanted to meet with the Labor & Deliver nurse again. I
continued to be incredibly nervous about a c-section and I wanted to learn more about what it would
entail. Our nurse was very excited to hear that Hannah was continuing to thrive in utero and was happy
to meet with us again. She had personally had 2 c-sections at this hospital, so she walked us through the
entire process from beginning to end. She warned me that the spinal may make it feel like I’m not
breathing, so don’t panic…if I can talk it means I’m breathing!
At this meeting we also met the neonatal nurse practitioner (NNP). Because we were delivering at a
smaller hospital, there wasn’t a neonatologist on duty all the time, but an NNP was always there. The
day we went up to the hospital to talk, the NNP on duty just happened to be the mother of a child with
skeletal dysplasia who was only expected to live a short time after he was born, but ultimately graced
them with 4 years of life. She was an incredible resource. She helped us understand what the
differences were between nasal prong oxygen, CPAP, and intubation. She took us through the NICU to
show us where Hannah might wind up. She told us stories of her beautiful son, giving us a glimpse into
life with a medically fragile child. Most importantly she told us “whatever decisions you make will be
the right decision, because you made it out of Love for your daughter”. These words were incredibly
soothing to me and have helped my through our entire journey with Hannah.
We had a follow up appointment coming up with our Palliative care doctor around 30 weeks. One of
the things she wanted us to think about was not providing a feeding tube if Hannah was unable to thrive
on bottle feeding or nursing alone. She had given us a paper that stated it was medically ethical to
withhold food in the case of genetic conditions such as trisomy 13 & 18. Even before reading the article
it felt wrong to us, and there was nothing in the article that changed our opinion. As with everything,
we asked ourselves “could we live with ourselves if we did or did not do x”. Not providing food was
something we would always regret and was immediately off the table. However we did temper it with
the statement that if Hannah could not digest the food and it cause her pain and discomfort we could
re-evaluate at that time. On the topic of chest compressions we were still divided and opted not to
make a decision about what we wanted quite yet. Also, as Hannah was proving to fight and stay strong,
as we continued down her path and didn’t see any structural issues that were life threatening, our
perspective on how we wanted her treated changed as well.
Earlier in our pregnancy we were really only looking for comfort care and to hold her the entire short time (we assumed) that we would have her. Now, with things continuing to look good…we wanted to make sure she had her best possible start in life. If that meant she needed to be in the NICU, we were ok with that, because we had full access to her in the NICU. If it meant she needed a test to evaluate her condition, we were ok with that. We still were not comfortable with intubation, because we couldn’t hold her. We wanted her declare for herself that she was strong and capable of sustaining life outside of the womb. We wanted to follow her lead. We presented much of this information to our palliative care doctor by email in the initial birth plan that we developed for Hannah. Because it held some fundamental shifts from our previous conversation our doctor had some very hard hitting, and at times abrasive-feeling questions for us. It was frustrating to have to justify the request for care that would be given to any other child. However, I knew that this doctor was our conduit to the neonatologist that would be caring for Hannah. It was in Hannah’s best interest to reply rationally and reasonably to her questions. I desperately needed her to not only support our decisions but to also stay on our “side”. I replied to each of her points calmly, professionally, and whenever possible with data either from journal articles or first-hand accounts. I wanted her to understand that we had realistic expectations for Hannah, but at the same time wanted to give her enough support that she could get established outside of the womb. We wanted Hannah to have a fair shot at declaring for herself that she was a survivor or if the world was just too much for her. Ultimately the doctor agreed with all of our points and agreed to support our decisions. We all agreed that at the core we all wanted what was best for Hannah and that it was good to fully flesh out all of our decisions, including asking the hard questions.
We continued to monitor Hannah’s heartbeat at home with our doppler twice a day ensuring it
remained fast enough. Then one evening at 32 weeks I watched it dip below the lower limit. Her heart
rate would be in a normal place, and then it would slow and stay there for a short while then come back
up. My heart dropped into my stomach. Naturally, this was also a night when my husband wasn’t
coming home until late, so it was just me. I drank some sugary coffee in hopes she just needed a little
stimulation. I checked her again and she stayed up where she was supposed to be. When my husband
came home that night we checked her again and she was still okay. However I was still scared. Luckily I
had an appointment with my OB the next day. I needed my doctor’s reassurance that Hannah was still
ok. When I explained to her what happened she decided we needed to do a Non Stress Test (NST) on
Hannah. This consisted of having 2 belts strapped to my pregnant belly. One to record Hannah’s
heartbeat, the other to record contractions. The nurse got me set up and then left my husband and I in
the room to listen to her heartbeat for 20 minutes. The doctor was looking for accelerations and
decelerations. What I had described to my doctor sounded like a deceleration which is a sign that the
baby is in distress. What we wanted to see what Hannah have at least 3 accelerations in the 20 minute
period. Which she did. She was just fine. However, at this point my doctor wanted to do an NST
whenever I saw her. It gave both her and I peace of mind that Hannah was continuing to do well.
Meanwhile, we continued to track Hannahs S/D ratio closely. We were getting weekly reads on her
umbilical cord blood flow as well as a bio physical profile (BPP). Usually a BPP consists of an NST and the
sonographer looking for the following 4 characteristics: practice breaths, movement, muscle tone, and
amniotic fluid level. Because my OB was performing the NST, the perinatologist only reviewed the 4
aspects that had to be seen on an ultrasound. I was especially concerned about the amount of amniotic
fluid. One of the life threatening complications of T18 is when the esophagus doesn’t connect to the
stomach (esophageal atresia). When this happens amniotic fluid builds up because it doesn’t process
through babies body in the normal fashion. This can also happen when there are significant issues with
the baby’s kidneys. Luckily Hannah’s fluid levels were on the higher end of normal, which meant it was
likely she didn’t have either issue, but probably had low muscle tone and just wasn’t as good at
swallowing the fluid as a typical baby would be. The best part about being tracked so closely is how
often we got to see Hannah. I loved how close we got to her in utero.
One of the things that worried me the most about delivery was respiratory distress. Would Hannah’s
lungs work? They don’t need to work in utero, so we really had no idea how they would do after birth. I
turned to the social networks and polled parents of children who had already been born. I asked them
“were your child’s lungs fully developed when they were born”? The answers I got back, especially from
parents whose children were born earlier than 38 weeks was worrisome. Even though typical babies
have fully developed lungs at 38 weeks, trisomy 13/18 kids didn’t. I had 3 different mothers tell me
their child’s lungs were not making surfactant. Surfactant is the slippery substance in the lungs that
helps the air sacks open and close smoothly, a substance critical to the ability to breathe. The good
news is there was something we could do about it, but it was outside of the norm. Moms that are in
danger of delivering before 34 weeks are given steroid shots that cause their baby to develop more lung
surfactant. But there was no benefit shown giving the shots later than 34 weeks. At this point I was
expecting to deliver at 37 weeks, but I based on my research, steroids would be beneficial to Hannah. I
spoke with both my OB and my perinatologist. They both felt there was minimal risk to Hannah and
myself and potentially a big upside to Hannah at birth, therefore they were willing to give me the
steroids.
Over the course of this pregnancy the team of medical professionals taking care of us was committed to
doing whatever we could to get Hannah here alive and at her peak potential. Now it was time to really
pull in the neonatologist, who was the doctor that was going to take care of Hannah once she was born.
I had the birth plan I’d worked through with our palliative care doctor and I needed to finalize it with the
neonatologist who would likely be present at her birth. This proved to be one of the hardest and most
gut-wrenching processes and it almost ended before it really even got going.
We gave the doctor a copy of our birth plan which we had already shared with the palliative care doctor,
and immediately hit a stumbling block when it came to chest compression. The doctor looked us in the
eye and told us that he would not perform chest compressions on Hannah. It pretty well stopped us in
our tracks. In retrospect I’m not sure why I wasn’t expecting it based on the conversation we’d
previously had with the palliative care doctor, but it was shocking to be told that our wishes would not
be followed based on the determination of this one man. We argued our point that chest compressions
only took a brief time and we wanted to give Hannah that chance, and he argued his point that if
Hannah needed chest compressions there were more significant issues than we were expecting and the
likelihood it was going to help would be small and the pain it would cause Hannah was high. After
discussing this issue for at least 5 minutes, my husband stated he wanted it to remain in the birth plan
and I looked at the doctors eyes and told my husband “we can keep it on this sheet of paper all we want,
but that doesn’t mean he will do it”. At that point I realized we had to move on otherwise we wouldn’t
get through any more of the plans that we needed to make. We in effect agreed to disagree on this
point and continued moving forward.
During the rest of the conversation we discussed many things. While we did not want to have Hannah
intubated, because we thought it would be painful and wouldn’t allow us to hold and cuddle Hannah
like we wanted to, we did want her to have CPAP support if she needed it. So one of the questions we
had to answer was how long should we have her on CPAP? In the back and forth conversation with the
neonatologist we decided that 7 days would be a good timeline. One of the common issues with
premature babies is Respiratory Distress Syndrome (RDS) which happens when the babies’ lungs haven’t
made enough surfactant. Even though I was planning to get a steroid shot to help Hannah produce
surfactant there were just too many unknowns. RDS tends to get worse after a day or two but then get
better around day 3-5. We decided that if Hannah was not showing enough improvement after 7 days
of being on the CPAP then it was likely due to an a physical anomaly, not RDS and it would not get better
in time, and therefore we should remove her from CPAP and allow her to pass. We wanted to give
Hannah the chance to declare for herself that she was capable of living outside of the womb, and this
was one of the biggest indications. Would she be able to breathe for herself? After being given a
window of opportunity to establish herself on the outside with a help from non-invasive CPAP, would
she be able to breathe on her own or with a little bit of nasal cannula oxygen? This would be key to her
declaring that she was strong enough.
The neonatologist was also in favor of minimizing the number of needle sticks on Hannah in order to
minimize any pain she would feel. We agreed that we did not want her to get the vitamin K shot or the
eye ointment treatment at birth, but were uncertain about what other needle sticks should or should
not be performed. One of my concerns was if she was jaundiced. The assured me they had a device
that could tell her bilirubin levels by taking a reading of her skin. We could use that as a guideline and if
it looked borderline we could always revisit the need to draw blood to check her it if we were worried. I
had asked about checking her carbon dioxide (CO2) level and if we needed test her blood gases. Based
on what I had learned from the parents on the support group, this test would indicate how well Hannah
was breathing. However, the doctor told me since she wasn’t on a ventilator we didn’t need to know her
blood gas, because that information is only used to adjust ventilator settings.
At this point our hour was up. I still had additional questions and we weren’t all the way through
Hannah’s birth plan. We agreed that we would all meet again on Monday of the next week. This delay
turned out to be a godsend because I had the opportunity to spend the weekend researching the
different issues that had arisen during our first meeting. Because Hannah was growth-restricted, I
researched the common issues for growth-restricted babies, going back to my trusty google.com
searching. Through this research I learned they tend to be hypoglycemic (low blood sugar) which can be
very easily corrected through ensuring proper milk intake or an IV of sugar water. I was also blessed to
attend church with a NICU nurse who works at the local children’s hospital and see the sickest of the sick
babies. I called her and had a very good conversation about all of the things that the doctor had told
me. It was so great to have someone I felt would give me the honest truth and could compare her
answers to my questions with what the doctor was telling me. She was also familiar with this
neonatologist and put me at ease that she would be confident with Hannah in his care. She said that he
was one of the best and most caring doctors that she worked with. Also, over the weekend my husband
and I talked at length about chest compressions. My NICU nurse friend confirmed what the
neonatologist said that if Hannah required chest compressions then we would likely be causing a lot of
pain with little hope of it helping her. I also remembered back to some personal accounts I had read of
children with different defects who never took a breath, but their heart beat for over an hour. Putting
all of that information together Jason and I realized that the reason we didn’t want intubation (it would
cause pain and keep her from our arms) is the exact same reason we shouldn’t want chest
compressions. It was a tough realization to come to, but we got there. I also realized that I should
respect the doctor for standing his ground by being upfront about his refusal to do chest compressions.
The next Monday at the final meeting, a couple more people were in the meeting. Not only did we have
the neonatologist and social worker who attended the last meeting but also the nurse from labor and
delivery who I’d been talking to all along and the nurse practitioner who would be there for the birth.
We started off talking about the chest compressions and that we had reached the same page the doctor
was on. We moved on to the rest of the birth plan and also talked about the growth restriction research
I had done over the weekend. This included the need to check Hannah’s blood after birth for
hypoglycemia and other issues that are common in newborns with trisomy 18. We talked about the
possibility or Hannah having central apnea issues whereby her brain would forget to tell her to breathe.
The neonatologist agreed to treat her with caffeine therapy (which is standard treatment for preemies
with central apnea) as well as providing nasal prong oxygen or CPAP, if needed. If Hannah was not able
to drink from a bottle either because she was not strong enough or because she aspirated (got milk into
her airway), they would provide a nasogastric tube (NG Tube) that goes in the nose to the stomach so
we could feed her. Throughout the discussion I stressed that I believed trisomy children are slower to
develop and needed support to transition from being in utero to the outside world, and that I wanted to
make sure we were giving Hannah that support and the time she needed to get her footing, even if it
meant time in the NICU or wearing a CPAP mask to help her to breathe. The labor and delivery nurse
asked me very pointedly “what if those days are the only days you have with her?” She meant that by
providing this treatment to Hannah, we could be missing out on time with her in our arms. This
question took my breath away because Hannah looked so good in utero and we didn’t see any heart
defect. The only thing we could see is that she was small I believed that she was going to be a survivor.
But I realized that because of the trisomy 18 diagnosis, I had to consider this possibility. I truly
appreciated the nurse making me think this through.
The nurse’s question forced us to evaluate all of the interventions with our ability to hold Hannah and
make sure we got the most out of all the time we had with her. We discussed the possibility that
Hannah would not be able to maintain her temperature since she weighed so little and agreed that
Jason and I would be able to hold her skin to skin with blankets if that’s what was called for as opposed
to having her in a warmer and out of our arms. We agreed that we would work to find a way for us to
hold her while getting bili light treatments for jaundice if that’s what she required. In effect the medical
staff and my husband and I agreed that we would do whatever we could from a minimally invasive
standpoint that would give Hannah the chance to know her family and the intense love we have for her
while giving her every opportunity to thrive. There was still a lot of fear with the interventions we had
agreed upon. What if she needed more? What if she could not come off of CPAP in 7 days. In that case
we would have to say goodbye to her without her ever leaving the NICU. But we wanted Hannah to
declare that she was strong enough for the world. We wanted her to tell us that she was a survivor. We
wanted to follow her lead.
Together with the neonatologist we developed a plan that all of us could support. Then the
neonatologist gave us one last surprise. He recommended that we not do anything that we just agreed
to. He told us that his recommendation was to hold her and love her for as long or as little time as we
would get with no medical intervention. He agreed to do everything we just talked though, but it was
his recommendation that we do none of it and just love on her. My husband and I smiled and nodded.
We said thank you, but we wish to pursue what we agreed to. We would be following Hannah’s lead and
supporting her as best we could as she transitioned to the world outside of the womb.
By 35 weeks everything was in place. All that was left was to wait for the appointed day. We scheduled
the c-section for a Monday morning, however I got a call from my OB on Sunday that there was no room
in the NICU and we were going to hold off delivery until Wednesday. Hannah had continued to look
good at all of the sonograms and NSTs so I was surprisingly calm about the delay and just enjoyed the
last few days of having Hannah with me.
On the day of her birth we went in to the hospital with a waiting room full of all the people that were
important for her to meet. After a couple hours of prep work in the labor room, I had to leave all of my
loved ones and walk with an L&D and an anesthesia nurse to the OR. I had been doing well but half way
through that walk it hit me that this was it. In a matter of minutes we were going to implement our
birth plan and learn if Hannah would be a survivor. Those sweet strangers held on to me as I cried and
gathered my strength to keep moving forward. We got to the OR and it slowly filled up with people
including my husband. My OB started the procedure. My husband was holding my hand. I started
humming…I have no idea what the tune was, but I know I kept saying something softly over and over
again. My doctor announced she was about to get to Hannah…and the next thing I heard was Hannah
cry.
That was 6 months ago and Hannah is still with us. She needed a little CPAP support for a day and a half
and to be tube fed, but we were able to take her home with us after 8 days in the hospital. The prenatal
journey was extremely challenging, but I believe without all of the effort we made to give our girl the
best opportunity to thrive, she would not be with us today.
We continue to stay in contact with many of the nurses that took care of us through the hospitalization
all of whom are overjoyed to see how well Hannah is doing. We even ran in to her neonatologist the
other day and were so excited to show him how that little bit of care in the beginning made all the
difference to keeping Hannah in the world. We hope that this positive experience with Hannah will help
all of her medical team be open and willing to intervene similarly for future trisomy babies.



























Recent Comments